[Healthcare\Medicine]
Callinan: “As the nation grapples to contain and treat patients with COVID-19, we’re rethinking how we care for people with other serious or terminal illnesses…medicine must adapt accordingly.”
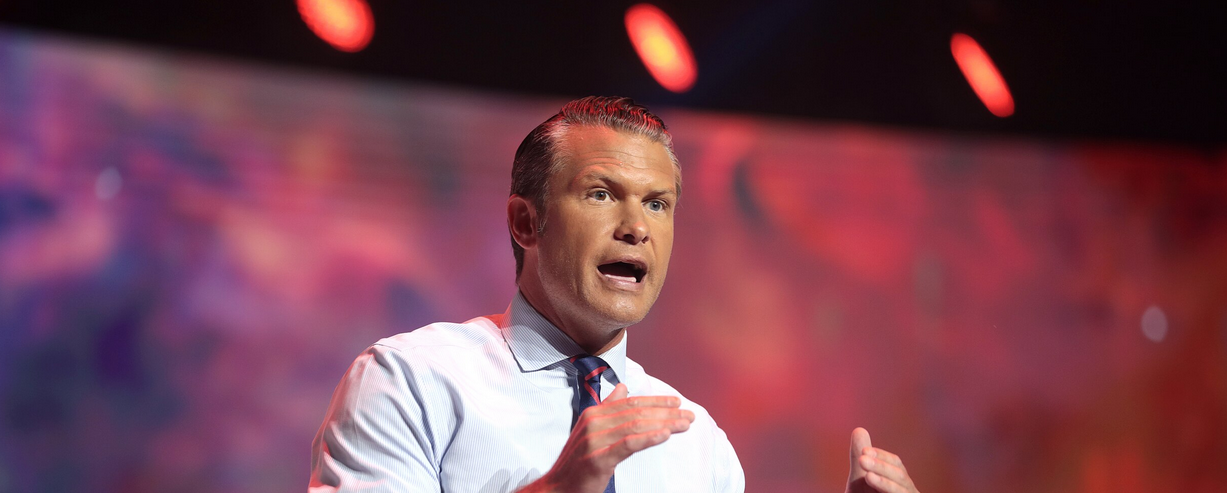
Photo: YouTube
Kim Callinan, President and CEO of Compassion & Choices says we must reimagine medicine and healthcare in America because of COVID-19.
“I have heart disease, and I am scared. For years, doctor’s visits and medication have kept me alive. However, now I am afraid if I go to the doctor, I will catch coronavirus and die. If I don’t go, my heart disease could kill me.”
I have had similar conversations with seriously ill Americans nationwide who have a host of diseases. They ARE legitimately at greater risk of dying prematurely if they are exposed to the coronavirus (COVID-19). Terminally ill patients at the end of their life face an even direr dilemma. They need access to quality medical care to control pain, manage symptoms, reduce suffering and extend their quality of life. A shortage of hospice care could drive them to seek pain and symptom management in already crowded, infectious emergency departments, which would increase their risk of a premature, painful death.
As the nation grapples to contain and treat patients with COVID-19, we’re rethinking how we care for people with other serious or terminal illnesses. Given that patients risk contracting the coronavirus at healthcare facilities designed to save lives, medicine must adapt accordingly, by replacing brick and mortar medicine with the safe, effective use of telehealth.
Fortunately, late last month the Centers for Medicare & Medicaid Services (CMS) issued regulations to implement telehealth provisions in the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) that significantly expand patients’ access to telehealth services. They will help ensure that vulnerable populations, including terminally ill patients, can seek care in the safety of their own homes while allowing quarantined doctors the ability to safely deliver quality health care.
These regulations include:
(1) CMS will now pay for more than 80 additional Medicare services when furnished via telehealth. They include emergency department visits, initial nursing facility and discharge visits, and home visits, which must be provided by a clinician that is allowed to provide telehealth.
(2) Providers can evaluate Medicare beneficiaries, who have audio phones only, a vitally important option for low tech seniors.
(3) Licensed clinical social worker services, clinical psychologist services, physical therapy services, occupational therapist services, and speech-language pathology services can receive payment for Medicare telehealth services.
(4) Licensed practitioners, such as nurse practitioners and physician assistants, are allowed to order Medicaid home health services during the existence of the public health emergency for the COVID-19 pandemic.
Fortunately, telehealth recently has become a rapidly growing care vehicle in the United States. According to a 2018 JAMA study, annual telehealth visits have increased at an average annual compound growth rate of 52 percent from 2005 to 2017. A 2018 study by Deloitte indicates that 9 out of 10 physicians recognize the benefits of telehealth. Furthermore, two-thirds of physicians (66%) note that virtual care improves patient access and the majority (52%) recognizes it improves patient satisfaction.
Despite these promising statistics and the new CARES Act provisions, widespread adoption of telehealth will take some time. It will require buy-in by both healthcare providers and patients to restructure our health system and make telehealth a first-line approach, particularly during the threat of COVID-19.
If you are a patient with a terminal or serious illness or a caregiver to one, talk with your healthcare providers about whether telehealth could replace an in person office visit. While it cannot substitute all office visits, it can be used in more instances than people realize. For example, clinicians are able to furnish patients with medical equipment so that they can monitor vital health indicators remotely and more effectively.
We know from experience that doctors are more likely to take the steps necessary to learn and then implement new approaches to medicine when patients request them. Given these facts, your self-advocacy for telehealth could benefit you, others, and ultimately contribute to more widespread and appropriate adoption.
Kim Callinan is President & CEO of Compassion & Choices.