Photos: YouTube
The New York City Health Department Monday released a new report emphasizing the need to address the root causes of smoking inequities, with recommendations on how to make progress. Although fewer adults in NYC smoke cigarettes than in decades past, some New Yorkers continue to smoke at higher rates, and smoking remains a leading cause of death. Smoking can cause heart disease, lung disease, stroke, diabetes, and over 10 types of cancers.
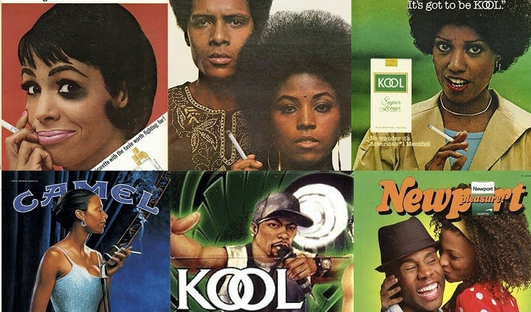
“Smoking kills and its inequitable impact is not accidental, it is by design,” said Health Commissioner Dr. Ashwin Vasan. “The tobacco industry has targeted marginalized people, mostly Black and Brown and low-income, for decades. They have done it locally and abroad. While they have reaped billions of dollars, New Yorkers have lost loved ones. These data bring the inequitable impacts of tobacco use into stark relief once again, and are a call to action to end the exploitation of our communities by Big Tobacco.”
The report includes data on the racist environmental and industry factors that can lead to inequities. They include disproportionate industry marketing and retailer access in communities with higher poverty and fewer protective factors, such as healthy coping resources or access to treatment support. For example, data are shown on menthol smoking rates, which highlight the harmful impact of aggressive tobacco industry promotion of menthol cigarettes to communities of color. In 2020, 52% of all adults who smoked in NYC usually smoked menthol cigarettes, but 89% of Black and 68% of Latino/a adults who smoked used menthol cigarettes, compared with only 32% of White and 25% of Asian/Pacific Islander adults who smoked.
The report also underscores the importance of acknowledging intersecting factors on smoking inequities. While overall smoking prevalence in NYC was similar across different race/ethnicity groups, considering race, ethnicity, gender, and nativity together revealed inequities. In 2019-2020, Asian/Pacific Islander men born outside the U.S. were more likely to smoke than U.S.-born Asian/Pacific Islander men (20% vs. 5%). The data tell a different story when looking at Black and Latino men, who were more likely to smoke if they were born in the U.S. (23% and 21%, respectively) than outside the U.S. (5% and 11%, respectively).
The report also examines tobacco treatment uptake and indicates that tailored outreach and treatment support must be prioritized. For example, Asian/Pacific Islander New Yorkers who smoke were less likely (9%) to have used nicotine replacement therapy (tobacco treatment medications used to manage nicotine cravings) than Black (24%), Latino/a (26%), and White (20%) adults who smoke, in 2016.
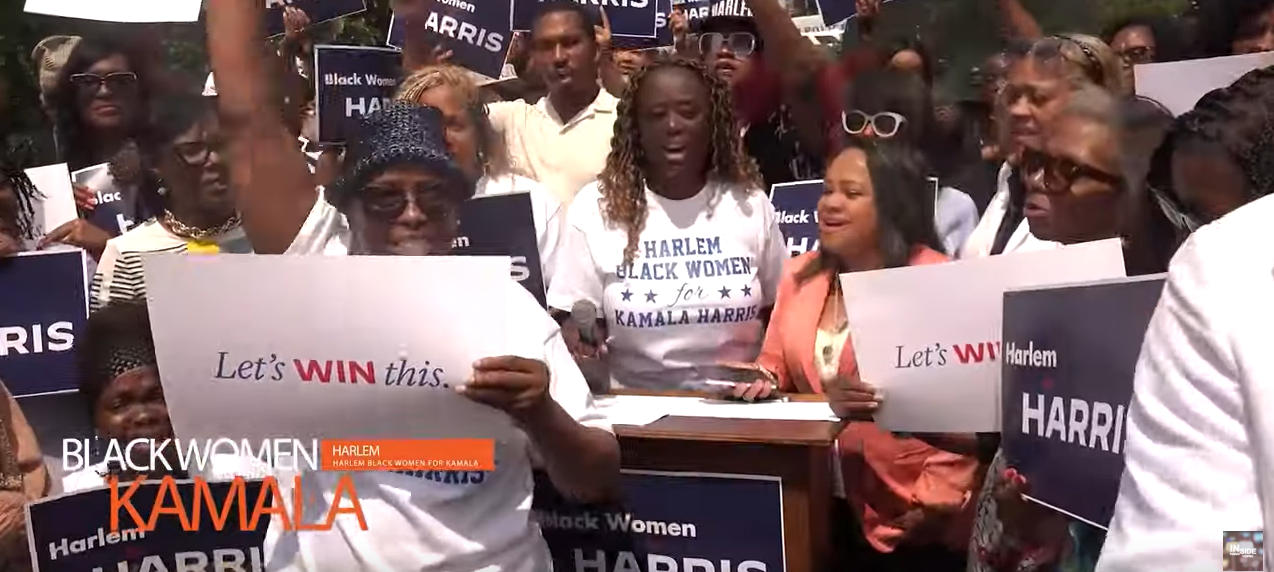
“We need to ensure that all communities are getting the support they need. Tobacco treatment medications and counseling can double someone’s chances of successfully quitting. Therefore, it is imperative that we work together to raise awareness about all the resources available to New Yorkers, such as the New York State Smokers’ Quitline or the Asian Smokers’ Quitline, the comprehensive Medicaid benefit and other insurance coverage for tobacco treatment, and numerous cessation programs across the city,” said Dr. Michelle Morse, the agency’s Chief Medical Officer and Deputy Commissioner of the Center for Health Equity and Community Wellness.
To support communities most impacted by smoking inequities:
Community-based organizations, public health practitioners, and social service providers can refer to the Race to Justice Action Kit for tips to communicate effectively and respectfully about health inequities and implement meaningful community engagement projects.
Clinicians should adopt best practices to address health inequities. Refer to the NYS Department of Health’s Health Care Organization Considerations In Support of Equity for tips.
Clinicians should screen all patients for tobacco use and offer tobacco treatment, including medications, to all patients who smoke, even if they are not ready to quit.
Researchers should apply anti-racism approaches to tobacco research and surveillance, including collecting and reporting disaggregated data when possible.
Public health advocates and policymakers should advocate for tailored solutions and policies grounded in equity that challenge industry influences, change unjust conditions, and break down barriers to community health.
Additional recommendations are available in the report. For more information on tobacco treatment resources, visit the NYC Quits webpage and Coping with Nicotine Withdrawal webpage. Clinical guidelines, tools, and resources are also available for clinicians.